Employers reap
healthcare savings by adding telemedicine to their portfolio of voluntary
benefits.
Each year, emergency departments provide valuable, life-saving care to millions of Americans. But many could be served better—and more cost-effectively—in an outpatient setting. In fact, misuse of U.S. emergency departments results in more than $30 billion
in preventable spending each year, according to research by the Agency for Healthcare Research and Quality[1].
And it’s not just the uninsured who are making unnecessary trips to the emergency department. A study by Truven Health Analytics found that 71% of the emergency room visits by patients with employer-sponsored insurance were for non-emergency conditions[2].
All of these avoidable visits are driving employers’ healthcare costs up to the point that so many are seeking a benefits solution that can redirect patients from emergency departments to appropriate outpatient settings. For a growing number of employers,
that solution is telemedicine.
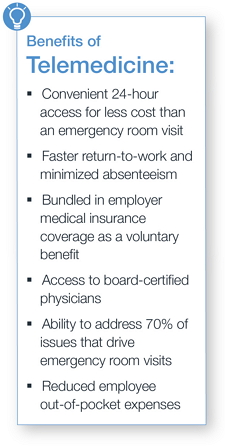 Telemedicine provides 24-hour access to board-certified physicians (via phone and video chat) who can diagnose and treat common illnesses and even prescribe short-term medication. Telemedicine provides the convenience of 24-hour care without the high price tag. Also,
because employees can access telemedicine on demand, without having to wait days or weeks for an appointment, it leads to faster resolution of medical issues leading to less absenteeism and increased productivity at the office.
Telemedicine provides 24-hour access to board-certified physicians (via phone and video chat) who can diagnose and treat common illnesses and even prescribe short-term medication. Telemedicine provides the convenience of 24-hour care without the high price tag. Also,
because employees can access telemedicine on demand, without having to wait days or weeks for an appointment, it leads to faster resolution of medical issues leading to less absenteeism and increased productivity at the office.
“A telemedicine program can be bundled into an employer’s medical insurance coverage or offered as a voluntary benefit,” said
Danny Talley, senior vice president, HUB International. “When included within the portfolio of voluntary benefits, telemedicine provides employees a user-friendly, value-driven benefit while simultaneously delivering cost savings to employers and
employees.”
Tackling obstacles to care
One reason people seek care from an emergency department or urgent care center is because the wait for a doctor’s appointment is so long. According to a survey by healthcare search and consulting firm Merritt Hawkins, the average time new patients wait to see a primary
care physician is 19.5 days[3].
For some people, the emergency room or urgent care center is the provider of choice because of its around-the-clock availability. A report released by the Centers for Disease Control (CDC) found that nearly half of people who visited an emergency department did so simply because the doctor’s office was not open[4].
Telemedicine tackles these obstacles to care by offering 24-hour access to physicians, and prompt response and callbacks, according to Talley. Typical telemedicine consultations include
cold and flu symptoms, bronchitis, respiratory infection, sinus problems, allergies, skin issues, pink eye and ear infections - the same issues that drive most emergency room and doctor visits. “Over 70% of these types of visits can be taken care of in a 15-minute phone call or video chat,” Talley
said.
A
comprehensive solution
 To help employers navigate telemedicine, HUB created
HUB Telehealth, a comprehensive voluntary benefits solution that brings together three telemedicine services into one package, including 24-hour access to medical doctors, personalized healthcare management and online access to medical experts. When offered as a voluntary benefit, employees pay a low per-month premium
(typically as low as $8/month/per person) no matter how many times employees call.
To help employers navigate telemedicine, HUB created
HUB Telehealth, a comprehensive voluntary benefits solution that brings together three telemedicine services into one package, including 24-hour access to medical doctors, personalized healthcare management and online access to medical experts. When offered as a voluntary benefit, employees pay a low per-month premium
(typically as low as $8/month/per person) no matter how many times employees call.
24-hour Access. Employees have access to a national network of board-certified doctors via phone or online video consultation. The average callback time is just 10 minutes, while for video consultations, members can pick and choose the day and time block that best fits their needs.
“You can show them a rash, pink eye, etc. All are common conditions that are easily diagnosable and treatable,” said Talley. “In fact, more than 90% of calls are able to be handled completely by the on-call physician, with no follow-up care necessary.”
Personalized
Healthcare Management. A confidential concierge service helps employees navigate the healthcare system and their health benefits. Advocates work with healthcare providers to lower the balance on any uncovered medical or dental bill over $400, and also can assist with scheduling appointments.
Online Access. With 24-hour access to credible online health information, employees simply log onto a secure site and submit their medical question. Within a few hours, they will receive an answer from an expert team of board-certified physicians.
“When we’re out doing our open enrollment meetings, we’re constantly telling the employees you need to be good consumers, don’t over-utilize the system,” said Talley. “Don’t use the ER when you can use urgent care, and don’t use urgent care when you can use the
doctor’s office. But when we leave these meetings, we never gave them a tool for how to do that. HUB Telehealth is now that tool.”
For more information on HUB Telehealth,
contact your HUB employee benefits consultant.
[1] Nationwide Frequency and Costs of Potentially Preventable Hospitalizations, 2006
[2] Study Find Most Emergency Room Visits Made by Privately Insurance Patients Avoidable
[3] Patient Wait Time, 2014
[4] CDC, Emergency Room Use